Patient safety and the advertising of vaccines to critical health and social care professionals are being discussed in England today.
- Ongoing discussions about immune system vaccination by future health care professionals.
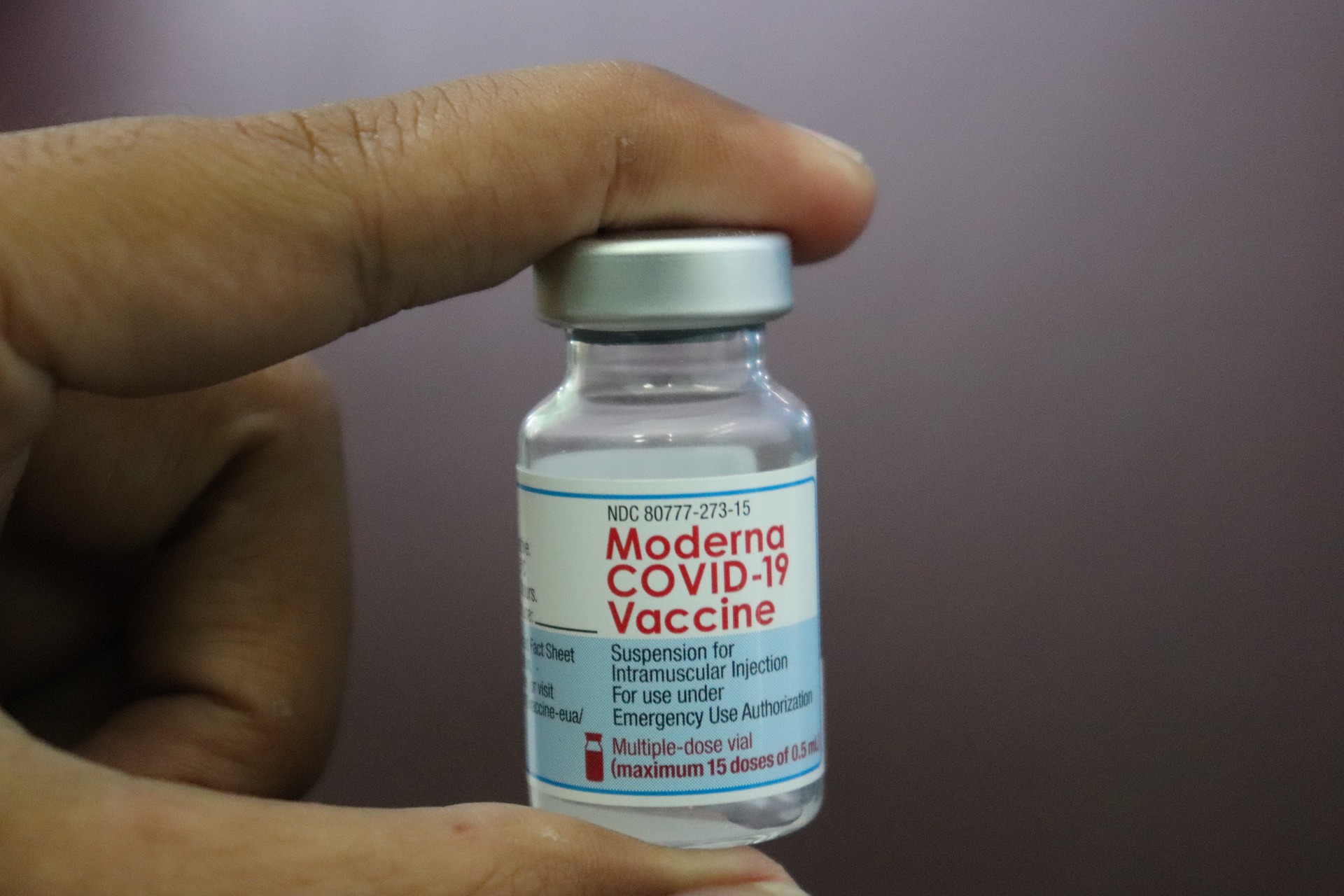
- Workers should be given the ECVID-19 and flu vaccination to protect patients from illness, serious illness, or death.
- 92% of NHS workers received their first injections and 88% of all vaccines were COVID-19 injections, while ministers called on everyone to take care of themselves and ensure safety.
The government is asking for insights into health programs and care facilities in England that require COVID-19 and flu vaccines to protect vulnerable people.
It takes six weeks to ask questions and see if health care providers and the general public are needed: those who interact with patients and those who receive help. This means that those who are fully vaccinated, if not treated, can be identified for the provision of treatment and care services. The purpose of the consultant is to imagine that a flu vaccine may be needed by health care professionals and workers.
NHS technology always has a module for protective pieces. The health care system has health and safety policies and regulations that require protection against hepatitis B from those who perform common procedures (e.g., surgeons).
The percentage of trusted NHS workers receiving a single dose of Covid is around 92% nationwide, with 88% of workers receiving all types. However, adoption circumstances vary and new information needs to be published showing that the adoption fee could range from 78% to 94% for all NHS-based categories.
The overall prevalence of influenza prevention increased from 14% in 2002 to 76% last year. However, in some cases, prices are as high as 53%.
The flu vaccine has been recommended for workers and vulnerable groups in the UK since 1960, with an average of more than 12,000 deaths a year in England between 2015 and 2020. In the winter of the year, 86% of the population aged 65 have flu illnesses.
In addition to protecting vulnerable patients, its use ensures the safety of workers, which is particularly important for reliable hospitals, where unplanned staff absences can speed up rapid work. Strong hospitals prepare patients for busy weather like winter.
Health and Welfare Secretary Sajid Javid said:
”The majority of patients treated in hospitals and elsewhere are exposed to COVID-19 vaccination infection, and we should do everything we can to prevent it.
”It is very clear to see the effects of respiratory drugs that some may reduce, so we are still trying vaccination COVID-19 antibiotics and the flu.
”We think carefully about the answers to the questions, but I still urge some inexperienced NHS people to think about vaccination – for their lives and those around them.”
The government recently discussed the need for COVID-19 vaccination for the elderly. To keep housekeepers, staff must be washed and dried by 11 November, when they are registered under the supervision of CQC England.
The Community Disaster Management Advisory Committee (SAGE) has also recommended the establishment of a scientific testing department to provide vaccination programs and support to the NHS, where patients are in care homes for infertility. between residents or patients and staff.
The COVID-19 vaccine has already had a major impact in reducing hospital admissions and deaths, and the UK Government Department of Health estimates that more than 112,000 people have been rescued so far.
The Joint Committee on Vaccination and Prevention (JCVI) has recommended being the first in the UK this winter to mediate SARS-CoV-2, along with other respiratory infections such as fever. This can be very helpful during the NHS winter, and many vulnerable people are expected to be hospitalized in the coming months.
The interview seeks answers to the use, size, and safety of potential employees and to reduce employee insecurity. The research will help policymakers tell how changes can be made and who can be released if the process improves. Employees, healthcare providers, co-workers, patients, and their families are encouraged to listen to their thoughts and wait for a decision this winter.
Since the launch of COVID-19 in December 2020, the Department for Health and Welfare has been working with NHS England to develop a medicine suitable for healthcare professionals and social workers. NHS England continues to provide hundreds of protective roots for COVID-19 to facilitate international operations and provide information to address the concerns of potential customers at any time. Workers receive safe and effective injections from different groups
For example, a wide range of international data shows that vaccines are safe and effective for at-risk groups, including pregnant women – a group we know can expect to be vaccinated. Thus, studies have shown that pregnant women can become seriously ill with COVID-19 and 98% of them are hospitalized because COVID-19 is not given but they are not pregnant. Two drugs. COVID -19 United Kingdom.
Every year, NHS organizations plan to make it easier for workers to be vaccinated against the flu and encourage workers to get vaccinated, for example by opening hospitals in the area. Admission to hospitals or 24-hour injections is easy.
We will continue to do everything we can to protect NHS patients and prevent them from entering the hospital. The $ 5.4 billion announced in support of the NHS over the next six months on Monday will cover £ 2.8bn in repairing workers ’infections and protecting patients from infections.
History
- The Board will publish this advice. Britain after that.
- The interview looks at three hospital-related risks and their mitigation with antiretroviral drugs: the hospital’s work phase among staff, patients, and visitors intolerance; and great danger.
- Some sick or sick people may seek the advice of a Green Paper or JCVI before vaccination to see a doctor, otherwise, they will be left alone. We are confident that all laws that allow medical care are prohibited. All future laws in the Green Paper on the Vaccination of Communicable Diseases (COVID-19: Green Paper, Chapter 14) and the JCVI apply to hospital care.